Bridging from Cells to Cognition in Autism Pathophysiology: Biological Pathways to Defective Brain Function and Plasticity
American Journal of Biochemistry and Biotechnology 4 (2): 167-176, 2008
Matthew P. Anderson, Brian S. Hooker and Martha R. Herbert
Departments of Neurology and Pathology, Harvard Medical School/Beth Israel Deaconess Medical Center, Harvard Institutes of Medicine, High Throughput Biology Team, Fundamental Science Directorate, Pacific Northwest National Laboratory, Pediatric Neurology/Center for Morphometric Analysis, Massachusetts General Hospital/Harvard Medical School, and Center for Child and Adolescent Development, Cambridge Health Alliance/Harvard Medical School
Abstract
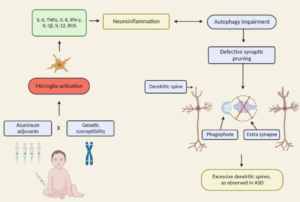
We review evidence to support a model where the disease process underlying autism may begin when an in utero or early postnatal environmental, infectious, seizure, or autoimmune insult triggers an immune response that increases reactive oxygen species (ROS) production in the brain that leads to DNA damage (nuclear and mitochondrial) and metabolic enzyme blockade and that these inflammatory and oxidative stressors persist beyond early development (with potential further exacerbations), producing ongoing functional consequences. In organs with a high metabolic demand such as the central nervous system, the continued use of mitochondria with damaged DNA and impaired metabolic enzyme function may generate additional ROS which will cause persistent activation of the innate immune system leading to more ROS production. Such a mechanism would self-sustain and possibly progressively worsen. The mitochondrial dysfunction and altered redox signal transduction pathways found in autism would conspire to activate both astroglia and microglia. These activated cells can then initiate a broad-spectrum proinflammatory gene response. Beyond the direct effects of ROS on neuronal function, receptors on neurons that bind the inflammatory mediators may serve to inhibit neuronal signaling to protect them from excitotoxic damage during various pathologic insults (e.g., infection). In autism, over-zealous neuroinflammatory responses could not only influence neural developmental processes, but may more significantly impair neural signaling involved in cognition in an ongoing fashion. This model makes specific predictions in patients and experimental animal models and suggests a number of targets sites of intervention. Our model of potentially reversible pathophysiological mechanisms in autism motivates our hope that effective therapies may soon appear on the horizon.