Excerpt:
“Our findings of significantly altered acylcarnitine levels in ASD support the hypothesis of altered fatty acid metabolism in a subset of ASD patients.”
Mitochondria
Small structures in a cell that are found in the cytoplasm (fluid that surrounds the cell nucleus). Mitochondria make most of the energy for the cell and have their own genetic material that is different from the genetic material found in the nucleus. Many diseases are caused by mutations (changes) in the DNA of mitochondria. Mitochondria are cell organelles. – NCI Dictionary of Cancer Terms, U.S. National Cancer Institute, 2021
Press Release from Harvard Magazine:
“Inflammation link for autism
A neuroimaging study has shown that the brains of young men with autism spectrum disorder have low levels of translocator protein, a substance that appears to play a role in inflammation and metabolism.
This discovery by a team of HMS researchers at Massachusetts General Hospital provides an important insight into the possible origins of autism spectrum disorder.
This developmental disorder, which affects one in fifty-nine children in the United States, emerges in early childhood and is characterized by difficulty communicating and interacting with others. Although the cause is unknown, growing evidence has linked it to neuroinflammation.
One sign of neuroinflammation is elevated levels of translocator protein, which can be measured in the brain using positron-emission tomography and anatomic magnetic resonance imaging.
The research team used these imaging tools to scan the brains of fifteen young adult males with the disorder. The group included both high- and low-functioning participants with varying degrees of intellectual ability. As a control, the team scanned the brains of eighteen non-autistic young men of similar age.
The scans showed that the brains of the young men with the disorder had lower levels of the protein, compared with the brains of non-autistic participants. In fact, those participants with the most severe symptoms of the disorder tended to have the lowest expression of the protein.
The brain regions found to have low expression of the protein have previously been linked to autism spectrum disorder and are thought to govern social and cognitive capacities such as processing emotions, interpreting facial expressions, and empathy.
The researchers point out that the translocator protein has multiple complex roles, some of which promote brain health. Adequate levels of the protein are, for example, necessary for normal functioning of mitochondria. Earlier research has linked malfunctioning mitochondria in brain cells to autism spectrum disorder.
Zürcher NR et al., Molecular Psychiatry, February 2020
Excerpt:
“The literature strongly supports that autism is most accurately seen as an acquired cellular detoxification deficiency syndrome with heterogeneous genetic predisposition that manifests pathophysiologic consequences of accumulated, run-away cellular toxicity. At a more general level, it is a form of a toxicant-induced loss of tolerance of toxins, and of chronic and sustained ER overload (“ER hyperstress”), contributing to neuronal and glial apoptosis via the unfolded protein response (UPR). Inherited risk of impaired cellular detoxification and circulating metal re-toxification in neurons and glial cells accompanied by chronic UPR is key.”
Abstract
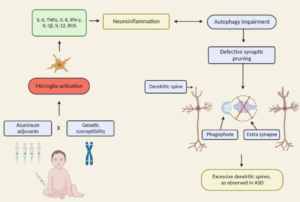
The conceptualisation of autistic spectrum disorder and Alzheimer’s disease has undergone something of a paradigm shift in recent years and rather than being viewed as single illnesses with a unitary pathogenesis and pathophysiology they are increasingly considered to be heterogeneous syndromes with a complex multifactorial aetiopathogenesis, involving a highly complex and diverse combination of genetic, epigenetic and environmental factors. One such environmental factor implicated as a potential cause in both syndromes is aluminium, as an element or as part of a salt, received, for example, in oral form or as an adjuvant. Such administration has the potential to induce pathology via several routes such as provoking dysfunction and/or activation of glial cells which play an indispensable role in the regulation of central nervous system homeostasis and neurodevelopment. Other routes include the generation of oxidative stress, depletion of reduced glutathione, direct and indirect reductions in mitochondrial performance and integrity, and increasing the production of proinflammatory cytokines in both the brain and peripherally. The mechanisms whereby environmental aluminium could contribute to the development of the highly specific pattern of neuropathology seen in Alzheimer’s disease are described. Also detailed are several mechanisms whereby significant quantities of aluminium introduced via immunisation could produce chronic neuropathology in genetically susceptible children. Accordingly, it is recommended that the use of aluminium salts in immunisations should be discontinued and that adults should take steps to minimise their exposure to environmental aluminium.
Excerpt:
“Environmental mercury is neurotoxic at doses well below the current reference levels considered to be safe, with evidence of neurotoxicity in children exposed to environmental sources including fish consumption and ethylmercury-containing vaccines. Possible neurotoxic mechanisms of mercury include direct effects on sulfhydryl groups, pericytes and cerebral endothelial cells, accumulation within astrocytes, microglial activation, induction of chronic oxidative stress, activation of immune-inflammatory pathways and impairment of mitochondrial functioning. (Epi-)genetic factors which may increase susceptibility to the toxic effects of mercury in ASD include the following: a greater propensity of males to the long-term neurotoxic effects of postnatal exposure and genetic polymorphisms in glutathione transferases and other glutathione-related genes and in selenoproteins. Furthermore, immune and inflammatory responses to immunisations with mercury-containing adjuvants are strongly influenced by polymorphisms in the human leukocyte antigen (HLA) region and by genes encoding effector proteins such as cytokines and pattern recognition receptors. Some epidemiological studies investigating a possible relationship between high environmental exposure to methylmercury and impaired neurodevelopment have reported a positive dose-dependent effect.”
Conclusion The literature reviewed here suggests a link between abnormalities in mitochondrial homeostasis and ASD and provides biochemical and genetic evidence to support a role for mitochondrial dysfunction in the pathogenesis of the autism phenotype.
Excerpt:
“Children who have (mitochondrial-related) dysfunctional cellular energy metabolism might be more prone to undergo autistic regression between 18 and 30 months of age if they also have infections or immunizations at the same time.”
Abstract
In this section, I explore the effects of mercury and inflammation on transsulfuration reactions, which can lead to elevations in androgens, and how this might relate to the male preponderance of autism spectrum disorders (ASD). It is known that mercury interferes with these biochemical reactions and that chronically elevated androgen levels also enhance the neurodevelopmental effects of excitotoxins. Both androgens and glutamate alter neuronal and glial calcium oscillations, which are known to regulate cell migration, maturation, and final brain cytoarchitectural structure. Studies have also shown high levels of DHEA and low levels of DHEA-S in ASD, which can result from both mercury toxicity and chronic inflammation. Chronic microglial activation appears to be a hallmark of ASD. Peripheral immune stimulation, mercury, and elevated levels of androgens can all stimulate microglial activation. Linked to both transsulfuration problems and chronic mercury toxicity are elevations in homocysteine levels in ASD patients. Homocysteine and especially its metabolic products are powerful excitotoxins. Intimately linked to elevations in DHEA, excitotoxicity and mercury toxicity are abnormalities in mitochondrial function. A number of studies have shown that reduced energy production by mitochondria greatly enhances excitotoxicity. Finally, I discuss the effects of chronic inflammation and elevated mercury levels on glutathione and metallothionein.
Abstract
Autism spectrum disorders (ASDs) are complex, heterogeneous disorders caused by an interaction between genetic vulnerability and environmental factors. In an effort to better target the underlying roots of ASD for diagnosis and treatment, efforts to identify reliable biomarkers in genetics, neuroimaging, gene expression, and measures of the body’s metabolism are growing. For this article, we review the published studies of potential biomarkers in autism and conclude that while there is increasing promise of finding biomarkers that can help us target treatment, there are none with enough evidence to support routine clinical use unless medical illness is suspected. Promising biomarkers include those for mitochondrial function, oxidative stress, and immune function. Genetic clusters are also suggesting the potential for useful biomarkers.
Excerpt: “A recent review assessed the research on physiological abnormalities associated with ASD (44). The authors identified four main mechanisms that have been increasingly studied during the past decade: immunologic/inflammation, oxidative stress, environmental toxicants, and mitochondrial abnormalities. In addition, there is accumulating research on the lipid, GI systems, microglial activation, and the microbiome, and how these can also contribute to generating biomarkers associated with ASD (45, 46).
Pathways are interconnected with a defect in one likely leading to dysfunction in others. Many metabolic disorders can lead to endpoints such as impaired methylation, sulfuration, and detoxification pathways and nutritional deficiencies. Mitochondrial dysfunction, environmental risk factors, metabolic imbalances, and genetic susceptibility can all lead to oxidative stress (47), which in turn leads to inflammation, damaged cell membranes, autoimmunity (48), impaired methylation (49), cell death (48), and neurological deficits (50). The brain is highly vulnerable to oxidative stress (51), particularly in children (52) during the early part of development (47). As environmental events and metabolic imbalances affect oxidative stress and methylation, they also can affect the expression of genes.”
Excerpt:
“This suggests certain individuals with a mild mitochondrial defect may be highly susceptible to mitochondrial specific toxins like the vaccine preservative thimerosal.”