Excerpts:
“As a result of these pieces of evidence (epidemiological, clinical and preclinical data) pointing to a potential causal association between early ABA (aluminum-based adjuvants) exposure and increased ASD risk, new hypotheses regarding neurological and immunological consequences of ABA-containing vaccines and novel clinical strategies (i.e., postponing of ABA-containing vaccines and replacement of ABAs with calcium phosphate are now being considered.“
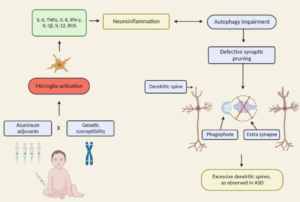
“Our review presents the lack of fundamental scientific data demonstrating that Al adjuvants are safe and do not induce any long-term side effects. It also supports further investigation related to the effects of early Al adjuvant exposures occurring in combination with genetic susceptibility factors, including autophagy, immune and inflammation process genes. As accumulating evidence shows that modulating the levels of autophagy may increase the risk of NDDs, such studies will elucidate a new etiology for these complex disorders and contribute to develop potential new diagnostic and therapeutic tools.”