The impact of neuroimmune alterations in autism spectrum disorder
Front. Psychiatry, 09 September 2015 Sec. Systems Biology Archive
Volume 6 – 2015 | https://doi.org/10.3389/fpsyt.2015.00121
The impact of neuroimmune alterations in autism spectrum disorder
Carmem Gottfried1,2, Victorio Bambini-Junior1,2,3, Fiona Francis4,5,6, Rudimar Riesgo1,7 and Wilson Savino3
1Translational Research Group in Autism Spectrum Disorder (GETTEA), Federal University of Rio Grande do Sul, Porto Alegre, Brazil
2Research Group in Neuroglial Plasticity, Department of Biochemistry, Federal University of Rio Grande do Sul, Porto Alegre, Brazil
3Laboratory on Thymus Research, Oswaldo Cruz Institute, Oswaldo Cruz Foundation, Rio de Janeiro, Brazil
4Sorbonne Université, Université Pierre et Marie Curie, Paris, France
5INSERM UMR-S 839, Paris, France
6Institut du Fer à Moulin, Paris, France
7Child Neurology Unit, Clinical Hospital of Porto Alegre, Federal University of Rio Grande do Sul, Porto Alegre, Brazil
Abstract
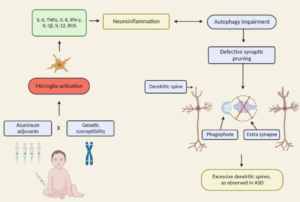
Autism spectrum disorder (ASD) involves a complex interplay of both genetic and environmental risk factors, with immune alterations and synaptic connection deficiency in early life. In the past decade, studies of ASD have substantially increased, in both humans and animal models. Immunological imbalance (including autoimmunity) has been proposed as a major etiological component in ASD, taking into account increased levels of pro-inflammatory cytokines observed in postmortem brain from patients, as well as autoantibody production. Also, epidemiological studies have established a correlation of ASD with family history of autoimmune diseases; associations with major histocompatibility complex haplotypes and abnormal levels of immunological markers in the blood. Moreover, the use of animal models to study ASD is providing increasing information on the relationship between the immune system and the pathophysiology of ASD. Herein, we will discuss the accumulating literature for ASD, giving special attention to the relevant aspects of factors that may be related to the neuroimmune interface in the development of ASD, including changes in neuroplasticity.
A commentary has been posted on this article:
GENERAL COMMENTARY article
Front. Psychiatry, 08 October 2015 Sec. Systems Biology Archive
Volume 6 – 2015 | https://doi.org/10.3389/fpsyt.2015.00145
Commentary: The impact of neuroimmune alterations in autism spectrum disorder
Dario Siniscalco 1,2,3*
1Department of Experimental Medicine, Second University of Naples, Naples, Italy
2Centre for Autism – La Forza del Silenzio, Caserta, Italy
3Cancellautismo – No Profit Association for Autism Care, Florence, Italy
The dramatic increasing prevalence of autism spectrum disorders (ASDs) (1), together with the influence on the quality of life and the lifetime societal cost of caring, has called for newest research on both the development of these diseases and the therapeutic options. Nowadays, it is well recognized that multifactorial and polygenic features (complex combination of genetic, epigenetic, and environmental interactions) characterize ASDs (2). Prenatal immune alterations and early inflammatory processes could be the autism etiological events. The authors Gottfried et al. (3) in this hypothesis-and-theory article discuss the recent findings in autism discovery. Starting from a brief historical way on autism development, the main topic of the article is to focus on the state-of-the-art of the novel findings in autism studies. The authors rightly highlight the newest challenging frontier of autism research: the neuroimmune axis alterations. These alterations are first evident in the cells early responsible for immune responses, as they are the precursors for macrophages, dendritic, and microglial cells: monocytes or peripheral blood mononuclear cells (PBMCs). These cells show strong dysfunctions in ASD children and are committed to a pro-inflammatory state, which in turn result in long-term immune alterations (4). In ASDs, altered PBMCs are responsible for elevated pro-inflammatory cytokine production. The up-regulation of inflammatory cytokines is also reflected in brain centers of autistic patients (5): the consequences are the induction of blood–brain barrier (the immunological interface between peripheral immune system and central nervous system) disruption. Changes in BBB permeability directly influence neural plasticity, connectivity and function, triggering impairments in social interaction, communication, and behavior (3). Immunological abnormalities also influence the gastrointestinal system and the microglial innate immune cells of the central nervous system (6). The authors also discuss the role of autoimmunity in the pathogenesis of autism. Familial or virus/bacteria-infected autoimmunity could be a risk factor for autism. Even if the exact cellular and molecular pathways responsible for the induction of neuroimmune alterations are still to be further clarify, a complex interaction among epigenetic and environmental risk factors (7) could trigger the neuroimmune abnormalities, such as abnormal neuron and glia responses.
Taken together, these autism-associated neuroimmune changes could help in identifying novel therapeutic target for a better future management of ASDs.