Excerpts:
“Herein, we will discuss the accumulating literature for ASD, giving special attention to the relevant aspects of factors that may be related to the neuroimmune interface in the development of ASD, including changes in neuroplasticity.”
Commentary on the article:
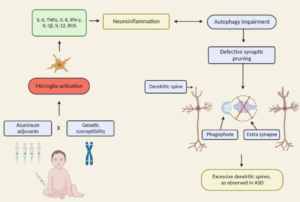
“The authors rightly highlight the newest challenging frontier of autism research: the neuroimmune axis alterations. These alterations are first evident in the cells early responsible for immune responses, as they are the precursors for macrophages, dendritic, and microglial cells: monocytes or peripheral blood mononuclear cells (PBMCs). These cells show strong dysfunctions in ASD children and are committed to a pro-inflammatory state, which in turn result in long-term immune alterations (4). In ASDs, altered PBMCs are responsible for elevated pro-inflammatory cytokine production. The up-regulation of inflammatory cytokines is also reflected in brain centers of autistic patients (5): the consequences are the induction of blood–brain barrier (the immunological interface between peripheral immune system and central nervous system) disruption. Changes in BBB permeability directly influence neural plasticity, connectivity and function, triggering impairments in social interaction, communication, and behavior (3). Immunological abnormalities also influence the gastrointestinal system and the microglial innate immune cells of the central nervous system (6). The authors also discuss the role of autoimmunity in the pathogenesis of autism. Familial or virus/bacteria-infected autoimmunity could be a risk factor for autism. Even if the exact cellular and molecular pathways responsible for the induction of neuroimmune alterations are still to be further clarify, a complex interaction among epigenetic and environmental risk factors (7) could trigger the neuroimmune abnormalities, such as abnormal neuron and glia responses.”