Examples of Outcome Reporting Bias in Vaccine Studies: Illustrating How Perpetuating Medical Consensus Can Impede Progress in Public Health
Cureus. 2022 Sep 21;14(9):e29399. doi: 10.7759/cureus.29399. eCollection 2022 Sep.
Gary S Goldman
Research, Independent Computer Scientist, Bogue Chitto, USA.
Abstract
Introduction: Outcome reporting bias in vaccine studies is a widespread problem among all researchers who have a tendency to report selective results and conclusions that support their beliefs and values or those of sponsoring agencies. Especially during the COVID-19 pandemic, this bias surfaced through the unprecedented proliferation of conflicting vaccine studies. Many researchers strongly recommend and report on the safety and effectiveness of the COVID-19 vaccine. Those researchers who embrace the COVID-19 vaccine and vaccines, in general, are often dismissive of other researchers who present views that differ from medical orthodoxy and oppose medical consensus.
Methods: The aim of this analysis is to critically evaluate seven vaccine studies using qualitative and/or quantitative approaches to identify outcome reporting bias and assess its potential impact on the stated conclusions that align with medical consensus. Four studies claim to have found no association between autism and (a) blood levels of mercury, (b) measles, mumps, and rubella (MMR) vaccine, and (c) thimerosal-containing vaccines. Three other studies claim no association exists between infant mortality rate and the number of vaccine doses, universal varicella vaccination and herpes zoster, and pandemic influenza vaccines and fetal losses.
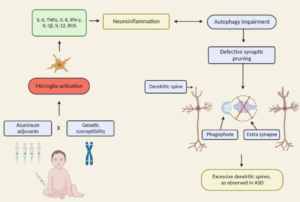
Results: The presence of outcome reporting bias and independent reanalysis demonstrated an impact on both the direction and magnitude of the observed effect – raising questions concerning the robustness of the original study design and conclusions and challenging the current medical consensus. Medical consensus has exonerated vaccines as having any causal relationship to autism spectrum disorders (ASDs), yet no other reasonable cause has been proposed. Medical consensus attributes significant ASD increases to better case ascertainment and broadened clinical diagnosis. According to 2018 data, an estimated 1 in 44 eight-year-olds has been identified with ASD. From 1990 to 2019, there have been an estimated two million new cases of ASD in the US, with lifetime social costs exceeding $7 trillion (in 2019 dollars). Can perpetuating medical consensus impede the advancement of public health? Or has it already done so?
Conclusions: Conflicts of interest (e.g., financial) that abound between health regulatory agencies and the pharmaceutical industry impact what is ultimately reckoned as medical consensus. Outcome reporting bias that is inherent to all researchers to some degree, obscures medical and scientific truth. Advancement of public health requires that researchers have integrity and an openness and willingness to collaborate to resolve contradictory findings. In fact, it is usually through meticulous, rigorous, scientific investigation of contradictory findings that medical science has advanced and contributed to improvements in public health – since medical consensus and orthodoxy can be incorrect.