Excerpts:
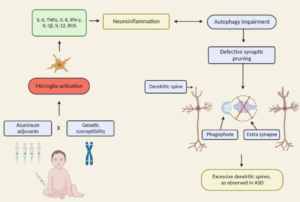
“In our clinical work and review of the literature, we have been impressed by the possible role of autoimmune disorders as influencing the pathophysiology of a distinct, objectively defined etiologic subtype of ASDs.”
“The notion that environmental factors contribute to ASD prevalence continues to evolve. Once-influential theories suggesting links among exposure to vaccines containing attenuated virus or toxins, conditions such as inflammatory bowel disease, and ASDs have fallen from favor since the retraction of a key study (Wakefield et al, 1998). It is important to emphasize, however, that the major reason for retraction was poor scientific method rather than theoretical flaws. Although ASDs are currently within the realm of psychiatrists and neurologists, it is becoming clear that at least some subtypes represent whole-body disorders, offering exciting new possibilities for therapy.”