Excerpt:
“Accumulating evidence implies the gut-brain axis as a pathway for MeHg harmful neurotoxic effects and a potential factor for later neurodegenerative disorders. The MeHg may induce a hormesis-related neuronal toxicity. Hormesis is an important redox dependent aging-associated neurodegenerative/ neuroprotective issue (Calabrese et al., 2010). The use of antioxidants, such as plant polyphenols (Calabrese et al., 2010; Leri et al., 2020) and protective nutrients (Oria et al., 2020) may be beneficial in reducing the MeHg-driven neuroinflammatory state and associated cell death with the interplay of the intestinal microbiota.”
admin
Excerpts:
“Aberrant migration of inhibitory interneurons can alter the formation of cortical circuitry and lead to severe neurologic disorders including epilepsy, autism, and schizophrenia.”
“These findings highlight key roles for JNK signaling in leading process branching, nucleokinesis, and the trafficking of centrosomes and cilia during interneuron migration, and further implicates JNK signaling as an important mediator of cortical development.”
“Background: Encephalitis, the inflammation of the brain, may be caused by an infection or an autoimmune reaction.”
“Conclusion: Gut microbiota disruption was observed in encephalitis patients, which manifested as pathogen dominance and health-promoting commensal depletion. Disease severity and brain damage may have associations with the gut microbiota or its metabolites.”
Excerpt
The data for these control tissues were compared with data (measured using identical procedures) for sporadic Alzheimer’s disease, familial Alzheimer’s disease, autism spectrum disorder and multiple sclerosis. Detailed statistical analyses showed that aluminium was significantly increased in each of these disease groups compared to control tissues. We have confirmed previous conclusions that the aluminium content of brain tissue in Alzheimer’s disease, autism spectrum disorder and multiple sclerosis is significantly elevated”
Press Release from Harvard Magazine:
“Inflammation link for autism
A neuroimaging study has shown that the brains of young men with autism spectrum disorder have low levels of translocator protein, a substance that appears to play a role in inflammation and metabolism.
This discovery by a team of HMS researchers at Massachusetts General Hospital provides an important insight into the possible origins of autism spectrum disorder.
This developmental disorder, which affects one in fifty-nine children in the United States, emerges in early childhood and is characterized by difficulty communicating and interacting with others. Although the cause is unknown, growing evidence has linked it to neuroinflammation.
One sign of neuroinflammation is elevated levels of translocator protein, which can be measured in the brain using positron-emission tomography and anatomic magnetic resonance imaging.
The research team used these imaging tools to scan the brains of fifteen young adult males with the disorder. The group included both high- and low-functioning participants with varying degrees of intellectual ability. As a control, the team scanned the brains of eighteen non-autistic young men of similar age.
The scans showed that the brains of the young men with the disorder had lower levels of the protein, compared with the brains of non-autistic participants. In fact, those participants with the most severe symptoms of the disorder tended to have the lowest expression of the protein.
The brain regions found to have low expression of the protein have previously been linked to autism spectrum disorder and are thought to govern social and cognitive capacities such as processing emotions, interpreting facial expressions, and empathy.
The researchers point out that the translocator protein has multiple complex roles, some of which promote brain health. Adequate levels of the protein are, for example, necessary for normal functioning of mitochondria. Earlier research has linked malfunctioning mitochondria in brain cells to autism spectrum disorder.
Zürcher NR et al., Molecular Psychiatry, February 2020
Excerpt:
“Results: A significant and positive correlation was found between hair metal burden (lead, aluminum, arsenic and cadmium levels) and severity of ASD symptoms (social communication deficits and repetitive, restrictive behaviors). Hair zinc level were inversely related with age while there was a negative, significant association between hair zinc level and severity of autistic symptoms (defective functional play and creativity and increase of stereotyped behavior). Lead, molybdenum and manganese hair levels were inversely correlated with cognitive level (full intelligence quotient) in ASD individuals.
Conclusions: The present study suggests the importance to combine metallomics analysis with pertinent disease features in ASD to identify potential environmental risk factors on an individual level possibly in the early developmental period.”
Discussion: The observation of predominantly intracellular aluminium in these tissues was novel and something similar has only previously been observed in cases of autism. The results suggest a strong inflammatory component in this case and support a role for aluminium in this rare and unusual case of CAA.
Except:
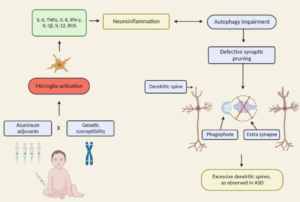
“There is a growing body of work to support the role of inflammatory cytokines in ASD. An emerging focus of research into the etiology of ASD has suggested neuroinflammation as one of the major candidates underlying the biologica model [5]. Plasma levels of IL-1β, IL-6 and IL-8 were increased in children with ASD and correlated with regressive autism, as well as impaired communication and aberrant behavior [6-8]. Vargas [9] showed an active neuroinflammatory process in the cerebral cortex, white matter, and in the cerebellum of autistic patients. Immunocytochemichal studies showed marked activation of microglia [5].”
Excerpt:
“Increased extra-axial cerebrospinal fluid (EA-CSF) have been observed in imaging studies of infant brains, who go on to develop autism. Folate deficiency can cause defects in neural development that can affect CSF production and drainage. Folate receptor alpha antibodies (FRAA) are observed in 75% of autism patients. Maternal FRAA have also been observed in the case of neural tube defects.
Folate deficiency can cause aluminum accumulation in the brain. Autistic brains have been shown to accumulate aluminum. FRAA in the child or mother can therefore explain all the observations”
Excerpt:
“This finding suggests that clinical events concerning neonatal IL-4 over-exposure, including neonatal hepatitis B vaccination and allergic asthma in human infants, may have adverse implications for brain development and cognition.”