Excerpt:
“The literature strongly supports that autism is most accurately seen as an acquired cellular detoxification deficiency syndrome with heterogeneous genetic predisposition that manifests pathophysiologic consequences of accumulated, run-away cellular toxicity. At a more general level, it is a form of a toxicant-induced loss of tolerance of toxins, and of chronic and sustained ER overload (“ER hyperstress”), contributing to neuronal and glial apoptosis via the unfolded protein response (UPR). Inherited risk of impaired cellular detoxification and circulating metal re-toxification in neurons and glial cells accompanied by chronic UPR is key.”
Inflammation
Abstract
Organic abnormalities with neuroinflammatory and psychiatric consequences involving abnormal kynurenine and purine metabolism, neurotransmitter and cytokine imbalances, and altered levels of nutrients and metabolites are noted in autism, and many of these abnormalities-specifically including increased intestinal permeability, microbial metabolites, and heightened serum levels of endotoxin-originate from the gut.
Abstract
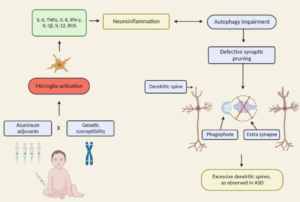
The conceptualisation of autistic spectrum disorder and Alzheimer’s disease has undergone something of a paradigm shift in recent years and rather than being viewed as single illnesses with a unitary pathogenesis and pathophysiology they are increasingly considered to be heterogeneous syndromes with a complex multifactorial aetiopathogenesis, involving a highly complex and diverse combination of genetic, epigenetic and environmental factors. One such environmental factor implicated as a potential cause in both syndromes is aluminium, as an element or as part of a salt, received, for example, in oral form or as an adjuvant. Such administration has the potential to induce pathology via several routes such as provoking dysfunction and/or activation of glial cells which play an indispensable role in the regulation of central nervous system homeostasis and neurodevelopment. Other routes include the generation of oxidative stress, depletion of reduced glutathione, direct and indirect reductions in mitochondrial performance and integrity, and increasing the production of proinflammatory cytokines in both the brain and peripherally. The mechanisms whereby environmental aluminium could contribute to the development of the highly specific pattern of neuropathology seen in Alzheimer’s disease are described. Also detailed are several mechanisms whereby significant quantities of aluminium introduced via immunisation could produce chronic neuropathology in genetically susceptible children. Accordingly, it is recommended that the use of aluminium salts in immunisations should be discontinued and that adults should take steps to minimise their exposure to environmental aluminium.
Excerpt:
“Environmental mercury is neurotoxic at doses well below the current reference levels considered to be safe, with evidence of neurotoxicity in children exposed to environmental sources including fish consumption and ethylmercury-containing vaccines. Possible neurotoxic mechanisms of mercury include direct effects on sulfhydryl groups, pericytes and cerebral endothelial cells, accumulation within astrocytes, microglial activation, induction of chronic oxidative stress, activation of immune-inflammatory pathways and impairment of mitochondrial functioning. (Epi-)genetic factors which may increase susceptibility to the toxic effects of mercury in ASD include the following: a greater propensity of males to the long-term neurotoxic effects of postnatal exposure and genetic polymorphisms in glutathione transferases and other glutathione-related genes and in selenoproteins. Furthermore, immune and inflammatory responses to immunisations with mercury-containing adjuvants are strongly influenced by polymorphisms in the human leukocyte antigen (HLA) region and by genes encoding effector proteins such as cytokines and pattern recognition receptors. Some epidemiological studies investigating a possible relationship between high environmental exposure to methylmercury and impaired neurodevelopment have reported a positive dose-dependent effect.”
INTERPRETATION:
Our findings suggest that predisposition to autoimmunity, and immune/inflammatory activation, may be associated with autistic regression.
Conclusions In the ASD brain, there is an altered expression of genes associated with BBB integrity coupled with increased neuroinflammation and possibly impaired gut barrier integrity.
Conclusions
In the ASD brain, there is an altered expression of genes associated with BBB integrity coupled with increased neuroinflammation and possibly impaired gut barrier integrity.
Abstract
Autism is a neurodevelopmental disorder characterized by deficits in communication and social skills as well as repetitive and stereotypical behaviors. While much effort has focused on the identification of genes associated with autism, research emerging within the past two decades suggests that immune dysfunction is a viable risk factor contributing to the neurodevelopmental deficits observed in autism spectrum disorders (ASD). Further, it is the heterogeneity within this disorder that has brought to light much of the current thinking regarding the subphenotypes within ASD and how the immune system is associated with these distinctions. This review will focus on the two main axes of immune involvement in ASD, namely dysfunction in the prenatal and postnatal periods. During gestation, prenatal insults including maternal infection and subsequent immunological activation may increase the risk of autism in the child. Similarly, the presence of maternally derived anti-brain autoantibodies found in ~20% of mothers whose children are at risk for developing autism has defined an additional subphenotype of ASD. The postnatal environment, on the other hand, is characterized by related but distinct profiles of immune dysregulation, inflammation, and endogenous autoantibodies that all persist within the affected individual. Further definition of the role of immune dysregulation in ASD thus necessitates a deeper understanding of the interaction between both maternal and child immune systems, and the role they have in diagnosis and treatment.
Excerpt: “Oxidative stress, brain inflammation, and microgliosis have been much documented in association with toxic exposures including various heavy metals…the awareness that the brain as well as medical conditions of children with autism may be conditioned by chronic biomedical abnormalities such as inflammation opens the possibility that meaningful biomedical interventions may be possible well past the window of maximal neuroplasticity in early childhood because the basis for assuming that all deficits can be attributed to fixed early developmental alterations in neural architecture has now been undermined.”
Excerpt:
“Levels of serum neurokinin A and BHg were measured in 84 children with ASD, aged between 3 and 10 years, and 84 healthy-matched children. There was a positive linear relationship between the Childhood Autism Rating Scale (CARS) and both serum neurokinin A and BHg. ASD children had significantly higher levels of serum neurokinin A than healthy controls (P < 0.001). Increased levels of serum neurokinin A and BHg were respectively found in 54.8 % and 42.9 % of the two groups. There was significant and positive linear relationship between levels of serum neurokinin A and BHg in children with moderate and severe ASD, but not in healthy control children. It was found that 78.3 % of the ASD patients with increased serum levels of neurokinin A had elevated BHg levels (P < 0.001). Neuroinflammation, with increased levels of neurokinin A, is seen in some children with ASD, and may be caused by elevated BHg levels. Further research is recommended to determine the pathogenic role of increased levels of serum neurokinin A and BHg in ASD. The therapeutic role of tachykinin receptor antagonists, a potential new class of anti-inflammatory medications, and Hg chelators, should also be studied in ASD."